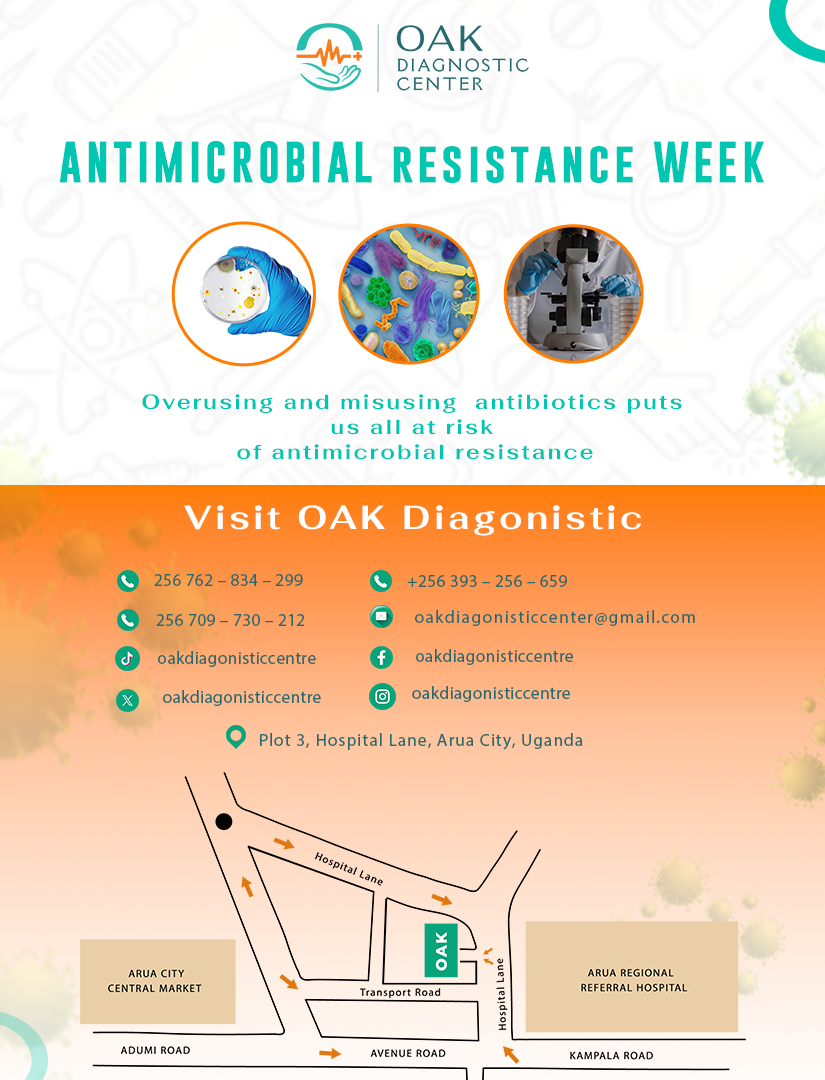
ANTIMICROBIAL RESISTANCE
Introduction
Antimicrobial resistance (AMR) is one of the pressing public health challenges facing the world today. The World Health Organization (WHO) warns that AMR is projected to become a leading cause of death globally by 2050 if significant action is not taken. As organisms evolve to resist the effects of medications, particularly antibiotics, the efficacy of existing treatments diminishes, leading to longer hospital stays, higher medical costs and increased mortality rates.
AR happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow. Resistant infections can be difficult, and sometimes impossible, to treat.
What is Antimicrobial Resistance?
Antimicrobial resistance occurs when microorganisms such as bacteria, viruses, fungi, and parasites evolve and develop the ability to withstand the effects of medications that once effectively treated them. The phenomenon can result from various factors including the misuse and overuse of antimicrobial drugs in humans and animals, inadequate infection prevention and control and poor sanitation and hygiene practices.
Causes of Antimicrobial Resistance
- Overuse and Misuse of antibiotics: The excessive use of antibiotics in humans and livestock accelerates the development of resistant strains.
- Poor infection prevention and control: Lack of proper hygiene and infection control in healthcare settings contributes to the spread of resistant strains
- Global spread: International travel and trade can hasten the spread of antimicrobial resistance across borders.
- Insufficient diagnostics: The absence of rapid diagnostic tools often leads to the misuse or inappropriate prescription of antibiotics.
- Self medication: In many parts of the world, individuals can purchase antibiotics without a prescription, leading to misuse and increased resistance.
The impact of antimicrobial resistance
World health Organization estimates that AMR causes at least 700,000 deaths globally each year. If no action is taken, this number could rise to 10 million by 2050.
The impact of AMR can result in:
- Prolonged stay in the hospital
- Higher medical costs
- Increased mortality rates
- Procedures such as surgery, cancer treatment become riskier in the presence of resistant infections
- Economic burdens on individuals and societies
Bacteria and fungi do not have to be resistant to every antibiotic or antifungal to be dangerous. Resistance to even one antibiotic or antifungal drug can mean serious problems. For example:
- Antimicrobial-resistant infections that require the use of second- and third-line treatments can harm patients by causing serious side effects, such as organ failure and prolong care and recovery, sometimes for months.
- Many medical advances are dependent on the ability to fight infections using antibiotics, including joint replacements, organ transplants, cancer therapy and the treatment of chronic diseases like diabetes, asthma and rheumatoid arthritis.
- In some cases, antimicrobial-resistant infections have no treatment options.
If antibiotics and antifungals lose their effectiveness, then we lose the ability to treat infections and control these public health threats.
How antimicrobial resistance happens
AR is a naturally occurring process. However, increases in antimicrobial resistance are driven by a combination of germs exposed to antibiotics and antifungals, and the spread of those germs and their resistance mechanisms.
How antibiotic and antifungal use affects antimicrobial resistance
Antibiotics and antifungals kill some germs that cause infections, but they also kill helpful germs that protect our body from infection. Antimicrobial resistance accelerates when antibiotics and antifungals pressure bacteria and fungi to adapt. The antimicrobial-resistant germs survive, multiply and spread to other germs. These surviving germs have resistance traits in their DNA that can spread to other germs.
Spread of germs and resistance mechanisms
To survive, germs can develop defence strategies against antibiotics and antifungals called resistance mechanisms. DNA tells the germ how to make specific proteins, which determine the germ’s resistance mechanisms. Bacteria and fungi can carry genes for many types of resistance.
Alarmingly, antimicrobial-resistant germs can share their resistance mechanisms with other germs that have not been exposed to antibiotics or antifungals.
5 things to know
- Antimicrobial resistance occurs when germs defeat the antibiotic or antifungal drugs designed to kill them. It does NOT mean your body is resistant to antibiotics or antifungals.
- Antimicrobial resistance can affect people at any stage of life. Infections caused by resistant germs are difficult—sometimes impossible—to treat. In many cases, these infections require extended hospital stays, additional follow-up doctor visits and treatments that may be costly and potentially toxic.
- Healthy habits can protect you from infections and help stop germs from spreading.
- Talk to your healthcare provider or veterinarian about whether antibiotics or antifungals are needed. Antibiotics and antifungals do not work on viruses, such as colds and the flu. These drugs save lives but can lead to side effects and antimicrobial resistance. If you have been taking these drugs, tell your doctor if you have three or more diarrhoea episodes in 24 hours.
- Tell your healthcare provider if you recently travelled to or received care in another country. Antimicrobial resistance has been found in all regions of the world. Modern trade and travel mean it can move easily across borders and can spread in places like hospitals, farms, the community and the environment.
Strategies to combat Antimicrobial Resistance
To tackle the growing threat of antimicrobial resistance, many initiatives have been put into place;
- Raising awareness: Enhance global understanding of antimicrobial resistance through effective communication, education, and training.
- Surveillance and research: Improve data collection on antimicrobial resistance to gauge the burden and formulate strategies for control.
- Infection prevention and control: Strengthen infection prevention and control measures, especially in healthcare settings.
- Antimicrobial stewardship: Promote the prudent use of antimicrobials in humans and animals to preserve the effectiveness of existing drugs
- Research and development: Encourage investments in new antibiotics, vaccines, diagnostics, and others
What can you do?
- Use antibiotics wisely: Only take antibiotics when prescribed by a healthcare professional, and complete the entire course, even if you feel better.
- Practice good hygiene: Regular handwashing, safe food preparation and proper sanitation can prevent infections and the spread of resistant bacteria
- Stay informed: Understand the issues surrounding antimicrobial resistance and educate others in your community
- Support policies and initiatives: Advocate for policies that promote responsible antibiotic use and better infection control practices
- Prevent infections in the first place.
- Improve antibiotic and antifungal use to slow the development of resistance.
- Stop the spread of antimicrobial resistance when it does develop.
- We all have a role to play, from travellers, animal owners and care givers to patients and healthcare providers.
Conclusion
Antimicrobial resistance is a global health crisis that demands immediate action from individuals, healthcare providers, policy makers and organizations. Combating antimicrobial resistance requires a collaborative and multifaceted approach, integrating education, policy reform, and scientific innovation. By understanding antimicrobial resistance and taking proactive steps, we can contribute to a healthier future and preserve the effectiveness of antimicrobial treatments for generations to come
REFERENCES: